Surgery for Endometriosis
Reviewed by: HU Medical Review Board | Last reviewed: March 2025 | Last updated: March 2025
Endometriosis can cause significant pain and disrupt daily life. When medicines or other therapies do not provide enough relief, surgery is often considered to treat endometriosis symptoms.1
Types of surgery for endometriosis
Doctors use different surgical approaches based on the severity and location of endometriosis. Each person’s case will be different. These surgeries include:1-3
- Laparoscopy – a minimally invasive approach
- Laparotomy – traditional open surgery
- Hysterectomy – removal of the uterus
Laparoscopy
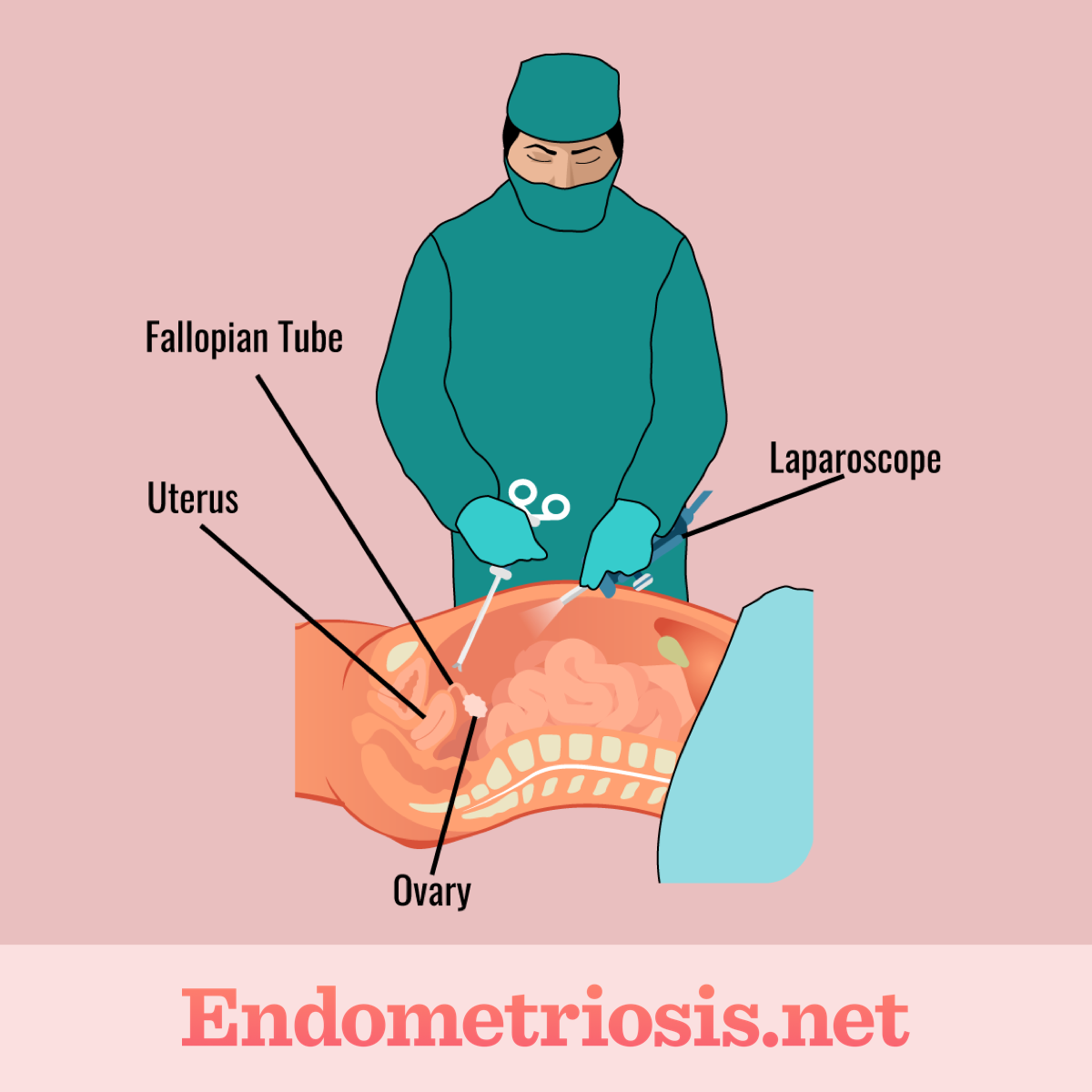
Figure 1. Laparoscopic surgery procedure
This is the most common surgery used to treat endometriosis. The surgeon makes a few small incisions in your abdomen. A laparoscope, a thin tube with a light and camera, is inserted to visualize the pelvic organs. Tiny surgical instruments are used to remove or destroy endometriosis tissue and scar tissue that is causing pain.1-3
Because laparoscopy is minimally invasive, there are many benefits, such as:1-3
- Smaller scars
- Less pain
- Faster recovery compared to traditional open surgery
Laparotomy
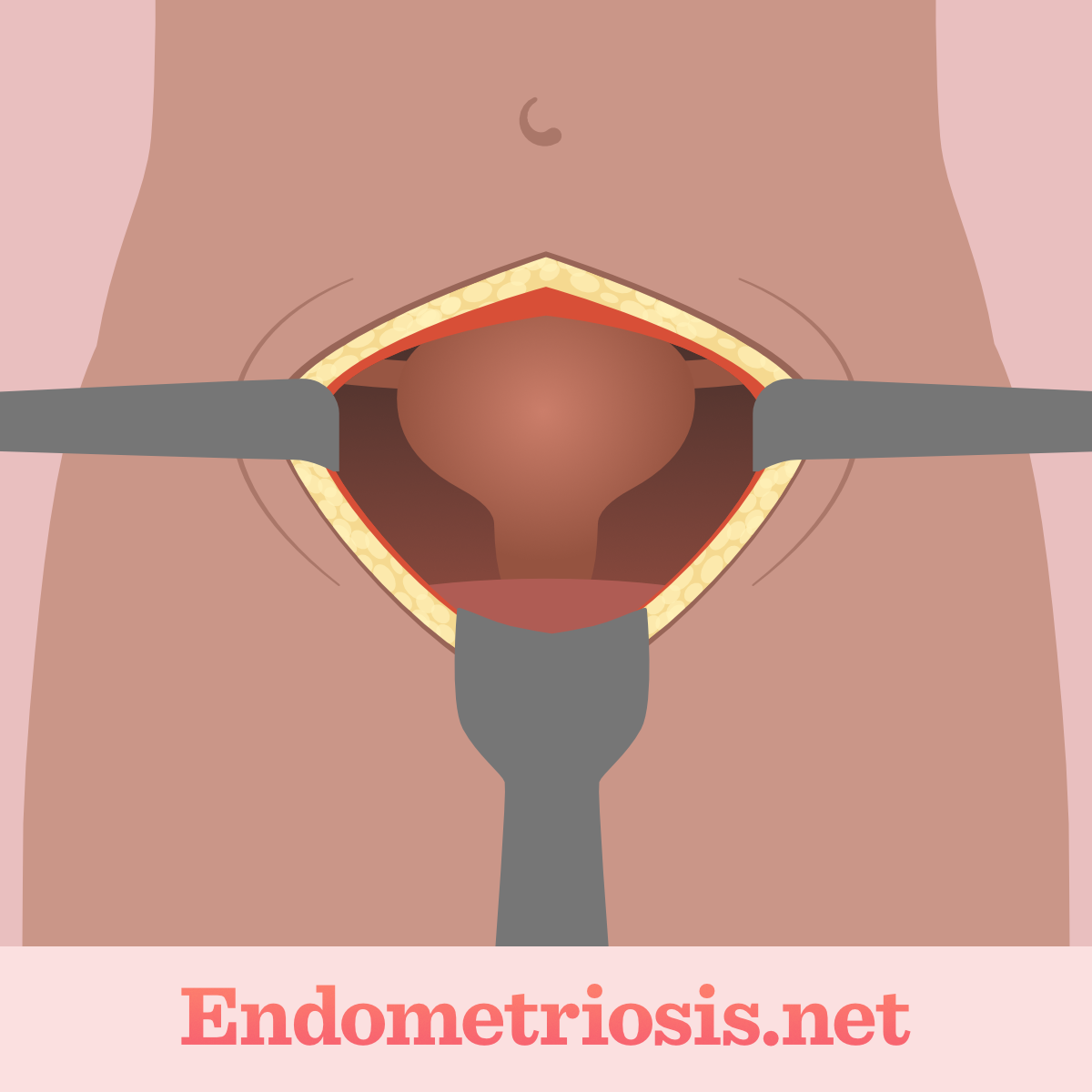
Figure 2. Laparotic surgery procedure
A laparotomy involves a larger incision in the abdomen. It is typically reserved for severe cases of endometriosis where extensive tissue removal is necessary.1-3
This approach may be required when endometriosis has spread to multiple organs or formed large cysts. This procedure is more invasive and has a longer recovery time.1-3
Hysterectomy
A hysterectomy is a surgical procedure where the uterus is removed. In some cases, the ovaries and fallopian tubes may also be removed.1-4
This is generally considered a last-resort option when other treatments have failed and when childbearing is no longer desired. A hysterectomy will cause you to no longer have menstrual periods or the ability to become pregnant.1-4
If you have endometriosis and are wanting to have children, talk with your doctor. There are fertility-preservation treatment options that can be considered.1
What to expect after endometriosis surgery
Recovery varies depending on the type of surgery. Here is what you can expect after the different procedures.2
After laparoscopy:2
- You may experience some pain and discomfort, which can be managed with pain medicine.
- You might feel bloated or have shoulder pain from the gas used during the procedure.
- Most patients can return home the same day or the next.
- Full recovery typically takes a few weeks.
After laparotomy:2
- Hospital stays are longer, usually several days.
- Pain management is crucial during recovery.
- Full recovery can take several weeks to months.
After hysterectomy:4
- Hospital stays range from a few days.
- Recovery involves managing pain and potential hormonal changes.
- Full recovery can take several weeks.
Risks associated with endometriosis surgery
Like any surgical procedure, endometriosis surgery carries potential risks. These can include:2,3
- Infection
- Damage to surrounding organs, such as the bowel, bladder, or ureters
- Scar tissue
- Bleeding
Can surgery cure endometriosis?
While surgery can greatly improve symptoms, it does not always guarantee a permanent cure. Surgery can remove visible endometriosis tissue, but microscopic implants may remain. Endometriosis can recur, especially if the underlying cause is not addressed.2,3
Hysterectomy is the most definitive surgical option. But it does not guarantee that all endometriosis will be gone, especially if it exists outside of the uterus.1,3,4
Hormonal therapies are often recommended after surgery to prevent recurrence. Generally speaking, the younger you are, the greater the likelihood of endometriosis recurring.1,3
Making informed decisions
If you are considering surgery for endometriosis:1,2
- Consult with a gynecologist specializing in endometriosis.
- Discuss your symptoms, medical history, and treatment goals.
- Understand the risks and benefits of each surgical option.
- Ask questions and get clarification on any concerns.
By being informed and working closely with your doctor, you can make the best decision for your individual needs.