Can a Urogynecologist Help My Bladder Pain?
I was diagnosed with interstitial cystitis(IC) about a decade ago. That's the medical term for bladder inflammation. My symptoms eventually lessened on their own, despite the lack of a treatment plan from my urologist and OB-GYN at the time. My bladder didn't exactly seem normal, but I didn't feel like I had a constant UTI anymore.
That is until I had a serious IC flare last fall. My pee pain was so bad it brought tears to my eyes. I hadn’t had a UTI in a decade. And since the at-home test was negative, I figured this was a sex-induced IC flare like the old days. I didn't know why my symptoms would show up then — was it pandemic stress? — but I treated the situation like I used to, with antihistamines, ibuprofen, and OTC bladder analgesics — the kind that turn your pee orange. I also stopped having intercourse for a of couple weeks, which is how long it took for my bladder to feel better.
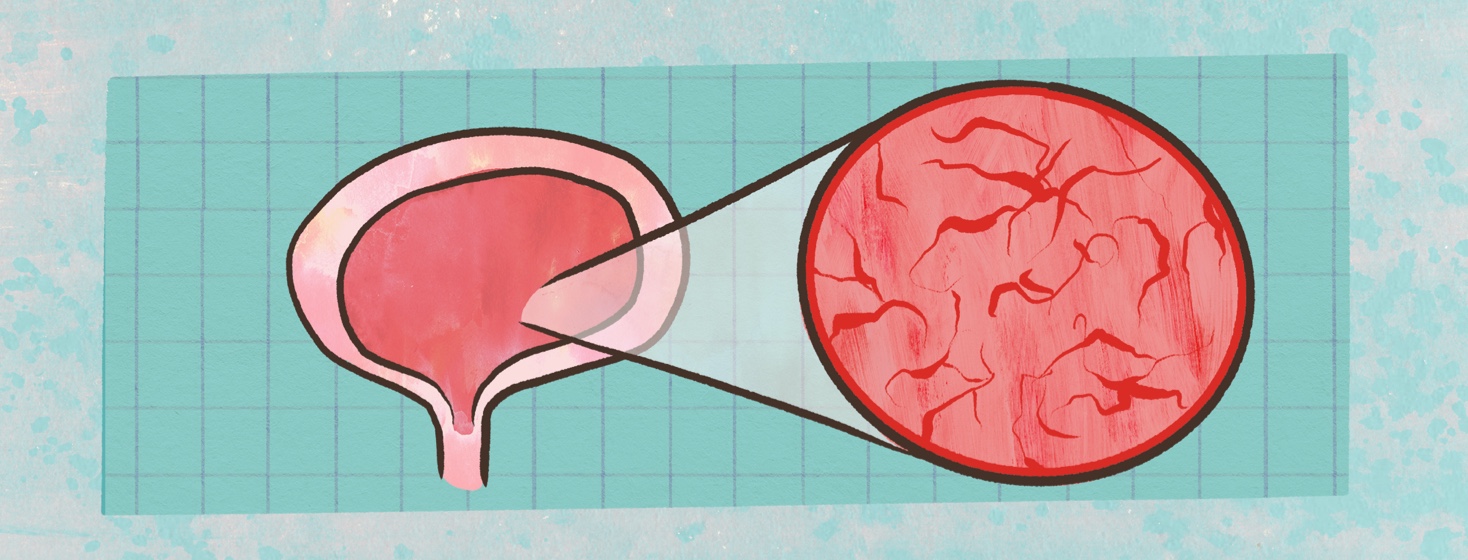
I immediately tried to get an appointment with an endometriosis and excision specialist who knew about IC, a visit I had to wait more than a half a year for. But, thankfully, I didn’t have another serious flare during that time. The surgeon didn't find endo on my bladder, but a cystoscopy — when they put a camera in your bladder — confirmed I had severe IC. And unlike the urologists of my past, he said, I needed to see someone who would know how to deal with it.
What Is a urogynecologist?
The doctor I saw technically specializes in female pelvic medicine and reconstructive surgery and urology. That's often referred to as urogynecology. He knows that people who have periods and give birth have specific issues that affect the bladder and urinary tract. This means they have a different approach to treatment for IC and more tools in their toolbox, if you will, compared to a general urologist.
The consultation and exam
I arrived with a full bladder, not an easy ask for someone with bladder sensitivity. The first thing I did was pee in a cup so they could check for signs of an infection. Like I expected, the culture was negative. In fact, the nurse told me my urine looked great, whatever that means. Then she took me into an exam room, checked my vitals, and scanned my pelvis with a fancy ultrasound tool I’d never seen before. It would measure how much pee was left in the bladder, she told me. They were looking to see if I had a problem emptying my urine. But other than my bladder sitting a little lower than average, everything looked normal.
After that, the doctor went over the pictures my endo surgeon gave me from my cystoscopy. He explained that all those burst blood vessels in my bladder lining aren't supposed to be there. Then he asked me a lot of questions, including:
- What triggers your IC?
- Do any foods or drinks make it worse?
- How long have you had these problems?
- Did your endometriosis surgeon find lesions on your bladder?
- How much do your symptoms interfere with your daily life?
- What are your goals with treatment?
- Have you tried any IC treatments before?
- Do any OTC and lifestyle changes help?
- Do any women in your family have bladder problems?
He did a pelvic exam after our chat, and he seemed very mindful of the fact that this can be uncomfortable for people with endo. (Though, it wasn't painful at all.) I had to cough so he could check for urine leakage. And he also looked for signs of prolapse, when the bladder drops into the vagina. I didn’t have any leaks or physical abnormalities, he told me.
The next steps for my treatment
He admitted that IC can be hard to manage. But there are several things we can try, he said. First, he gave me the OK to take OTC bladder analgesics for several days when I have a flare, which, for me, can happen after sex or before my period. He also wants me to do the following:
- Get a pelvic MRI to check for any cysts around my urinary system
- Start pelvic floor therapy again, this time with someone who specifically works on muscle tightness and bladder and pelvic pain
- Get a test to rule out some other infections
- Consider bladder instillation
Since bladder analgesics help, he thinks the bladder instillation is the most logical next choice. This is how that procedure works: They insert a catheter and fill your bladder with a solution, or wash, of dimethyl sulfoxide (DMSO). That's the only FDA-approved medicine for IC. It can lessen inflammation and relax bladder and pelvic muscles. You hold it for 10 or 15 minutes and then pee it out. It won't cure IC, but it can do a pretty good job of managing symptoms for some people, he told me.
I'll see my doctor again in six months to follow-up. And I'll keep you updated on my progress in the meantime.
Join the conversation